How do I talk to my patients and clients about … ?
 “Peter has been talking more and more. He reports improvement in mood and has been asking me more questions. How do I talk to him about diabetes?” Kate was enthusiastic with these questions to Roger, who happily responded, “I can see the change. Peter appears to be feeling better, and you are feeling good about your work with him. Let us now start talking about the best way to help him understand his conditions, including his diabetes.”
“Peter has been talking more and more. He reports improvement in mood and has been asking me more questions. How do I talk to him about diabetes?” Kate was enthusiastic with these questions to Roger, who happily responded, “I can see the change. Peter appears to be feeling better, and you are feeling good about your work with him. Let us now start talking about the best way to help him understand his conditions, including his diabetes.”
In the two previous articles, I reviewed why it is crucial to have Basic Integrated Care skills as a non-medical staff, and I explored the 10 most common reasons why your patients or clients are likely to die. In this current article, like Roger promised Kate, I am going to delve into how to best talk to your patients and clients about 5 of the 12 most common physical health conditions.
Obesity

Obesity is a medical condition characterized by an excess of body fat accumulation, and it contributes to the majority of the 10 leading causes of death discussed in a previous article, The Likelihood of Death: The 10 Reasons Why. Obesity affects 36% of Americans and is a risk factor for sleep apnea, osteoarthritis, cancer, depression and other comorbidities.
The body mass index (BMI), also known as the Quetelet index, tells whether a person’s weight is appropriate (the right proportion) for his or her height. The units for BMI measured are expressed as Kg/m2 (kg for weight and m2 for height). The normal values range between 18.5 and 25, while anything lower than 18.5 is considered underweight, within 25-30 is considered overweight, and anything over 30 is considered obese.
Like all other conditions, a combination of genetic vulnerability and environmental factors influence obesity. The environmental elements include limited physical exercise and excessive food intake. Moreover, some medications, like the newer antipsychotics and some physical health conditions, like hypothyroidism can contribute to obesity. This also means we can help our patients and clients prevent or manage obesity though lifestyle modifications, including exercise and healthy dieting. Decreasing the intake of foods high in fat and sugar and increasing the consumption of foods high in fiber and moderate in protein may lead to significant positive outcomes.
Lastly, when you talk with your patients and clients about obesity, be sensitive to possible stigmas. It is also important to ask about their views on obesity. In some cultures, for example, obesity is still seen as a symbol of prosperity and fertility; a conversation around these and other related beliefs is essential before beginning with any form of health education. As I mentioned in our previous article: 10 Tips to help engage your patients and clients, remember to “meet them where they are at.”
Hypertension
The most common cardiovascular disease (heart disease), hypertension, also known as high blood pressure, occurs 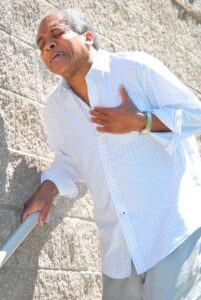 when the pressure of the blood in the arteries (blood vessels) is continuously high. It silently affects about 34% of Americans, until it becomes long term with complications. Uncontrolled hypertension is a major risk for other cardiovascular diseases, like coronary artery disease (CAD), Myocardial infarction (MI or heart attack), and heart failure. It also influences other conditions affecting other parts of the body and is considered a risk factor for cerebrovascular disease (stroke) and vision loss. As you may now know, both genetic and environmental factors are responsible for hypertension, and one area you can help your patients and clients is in lifestyle modification. Excessive salt intake and alcohol consumption, as well as smoking, in addition to being overweight or obese are major environmental risk factors for hypertension. I can’t emphasize enough the beneficial role of exercise in lowering blood pressure for your patients or clients and minimizing the risk for other medical complications. If your patient or client were to die today, there is an 18% chance that hypertension would be one of the contributing factors. Start talking with them about hypertension, what they can do about it and how intervention can make a difference in quality of life.
when the pressure of the blood in the arteries (blood vessels) is continuously high. It silently affects about 34% of Americans, until it becomes long term with complications. Uncontrolled hypertension is a major risk for other cardiovascular diseases, like coronary artery disease (CAD), Myocardial infarction (MI or heart attack), and heart failure. It also influences other conditions affecting other parts of the body and is considered a risk factor for cerebrovascular disease (stroke) and vision loss. As you may now know, both genetic and environmental factors are responsible for hypertension, and one area you can help your patients and clients is in lifestyle modification. Excessive salt intake and alcohol consumption, as well as smoking, in addition to being overweight or obese are major environmental risk factors for hypertension. I can’t emphasize enough the beneficial role of exercise in lowering blood pressure for your patients or clients and minimizing the risk for other medical complications. If your patient or client were to die today, there is an 18% chance that hypertension would be one of the contributing factors. Start talking with them about hypertension, what they can do about it and how intervention can make a difference in quality of life.
Arthritis
 Arthritis, which affects 23% of Americans, is the inflammation of the joints, causing pain, stiffness, and eventual destruction of joints. Other symptoms that may occur are redness in the affected joint area, warmth, and limited range of motion. The 3 most common forms of arthritis are Osteoarthritis, which is degenerative, Rheumatoid arthritis, and Gout. Arthritis is overall the most common cause of disability and tends to affect the fingers, knees, and feet. Relief from arthritis is an additional benefit you can mention to encourage your patients and clients to exercise and lose weight. Lastly, pay attention to the chronic pain associated with arthritis. Pain is an added risk factor for suicide, as I mentioned in the previous article.
Arthritis, which affects 23% of Americans, is the inflammation of the joints, causing pain, stiffness, and eventual destruction of joints. Other symptoms that may occur are redness in the affected joint area, warmth, and limited range of motion. The 3 most common forms of arthritis are Osteoarthritis, which is degenerative, Rheumatoid arthritis, and Gout. Arthritis is overall the most common cause of disability and tends to affect the fingers, knees, and feet. Relief from arthritis is an additional benefit you can mention to encourage your patients and clients to exercise and lose weight. Lastly, pay attention to the chronic pain associated with arthritis. Pain is an added risk factor for suicide, as I mentioned in the previous article.
Diabetes

I started describing Diabetes in a previous article – Likelihood of Death: The 10 Reasons Why. It affects 9% of the US population and is the top reason why your patients and clients may end up with renal (kidney) failure, lower limb amputation, and blindness. It can take ten or even twenty years, after diagnosis, for the complications of diabetes to develop, making it a silent disease. But this also means that prevention is key. The risk for diabetes can decrease by 28% with engagement in daily exercise of 90 minutes. Help your patients and clients start slow and find different strategies to begin and adhere to an exercise regimen. The most challenging part is to start, but once they begin, it will become increasingly easier and rewarding. In addition to exercise, a diet rich in whole grains, fiber, nuts, vegetables, and seafood can also help prevent and control diabetes. Avoiding red meats, sugar rich foods, and sodas and taking steps to stop smoking can also lead to significant positive results.
Hypothyroidism
Affecting 5-9% of the US population, hypothyroidism is a condition characterized by inadequate thyroid hormone,  which are responsible for regulating the body’s metabolism. It is commonly known as low thyroid or underactive thyroid and can cause a variety of signs and symptoms, including and not limited to constipation, weight gain, cognitive impairment, and depression. It can be caused by either limited iodine, or immune dysfunction, known as Hashimoto’s Thyroiditis, or injury in certain parts of the brain, previous treatment with radioactive iodine, or inadvertently by thyroid surgery. A mild form of hypothyroidism, known as subclinical hypothyroidism is common in the US, and it tends to affect more women than men. Subclinical hypothyroidism can be the cause of psychiatric symptoms, as explained in previous articles: Symptom Contextualization: Introducing A New And Key Concept; and Psychosis-Symptom Contextualization. Fatigue, depression, memory impairment, and low levels of motivation in your patients and clients may be due to hypothyroidism, for which treatment is readily available.
which are responsible for regulating the body’s metabolism. It is commonly known as low thyroid or underactive thyroid and can cause a variety of signs and symptoms, including and not limited to constipation, weight gain, cognitive impairment, and depression. It can be caused by either limited iodine, or immune dysfunction, known as Hashimoto’s Thyroiditis, or injury in certain parts of the brain, previous treatment with radioactive iodine, or inadvertently by thyroid surgery. A mild form of hypothyroidism, known as subclinical hypothyroidism is common in the US, and it tends to affect more women than men. Subclinical hypothyroidism can be the cause of psychiatric symptoms, as explained in previous articles: Symptom Contextualization: Introducing A New And Key Concept; and Psychosis-Symptom Contextualization. Fatigue, depression, memory impairment, and low levels of motivation in your patients and clients may be due to hypothyroidism, for which treatment is readily available.

“Peter has been talking more and more. He reports improvement in mood and has been asking me more questions. How do I talk to him about diabetes?” Kate asked Roger these questions. Then she followed with, “I am going to start working with Peter on an exercise regimen.”
Kate is curious and caring, consistently asking questions, learning, and implementing, step by step. You, too, are curious; you care and are working daily to make a difference in the lives of your patients and clients. Which of the above components do you plan to start implementing, today, in your practice?
Kindly share this article with your colleagues. Feel free to also share your story and experiences with me. As usual, thank you for allowing me to accompany you on this challenging, though noble and gratifying journey.
Remember: “A journey of a thousand miles begins with a single step.”
Start small, reach out, and together, we shall continue to make a difference in the lives of our patients and clients, particularly the vulnerable population we care for.