Violence Risk Assessment: What it Really Entails
“This patient is high risk for violence. His chart needs to be flagged,” said Danielle, the supervisor. “Done. What’s next? How do we proceed?” asked Dan, the clinician, who reported that he flags at least one to two patients on a daily basis, without any follow up or plans for next steps.
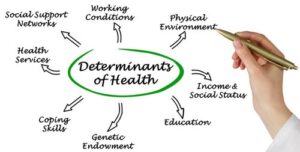
Violence risk assessment is conducted through clinical analysis and using instruments as auxiliaries. The LSCMI and HCR20* are some appropriate tools for use, though I must emphasize the need to always consider your case from a comprehensive viewpoint, to determine best practices and the right tool for immediate decision making. Unlike the historical factors, the contextual and clinical factors contributing to violence and recidivism can be influenced and changed, and they are to remain the clinician’s main focus. Given the now adequate data on the importance of addressing substance use and social determinants of health, all service plans for all individuals flagged as “high risk” need to prioritize targeting these factors as part of a mitigating strategic plan. Additional factors to be taken into consideration for deciding the best service plan in response to a “high risk” assessment determination, based on clinical appraisal and assessment tools are: age, crime severity, first time or repeat offense, and level of amenability to treatment.
While additional tools might help with the implementation of this decision making process, a multidisciplinary team-based discussion around making this decision is a crucial part of this approach. It is well known that the tools do not replace sound clinical judgment, but using these in combination—team discussion, sound clinical judgment and best tools—for immediate decision-making is a better method when working with any high-risk population. Such a process ensures the provided services are tailored and individualized, comprehensive and recovery promoting, not simply based on a “one size fits all” approach.
Other factors to take into consideration as part of a decision-making process include: (1) addressing the social determinants of health and (2) minimizing the likelihood that an individual will return to a high-crime neighborhood or continuing to associate with the same types of peers.
continuing to associate with the same types of peers.
Advocating for placement in a supervised setting may therefore be necessary for some. Further, all attempts are to be made to help individuals with structured time, and, whenever possible, an engagement strategy is required and must involve the individual’s family members and other members of his or her community. Such an engagement strategy will include a plan to promote medication adherence and improve show rate to the mental health provider, substance use and other level of functioning promoting programs. Lastly, a coping skills promoting group are to be part of a service plan for those at risk for violence and recidivism. Since trauma is often undiagnosed in this population—one with a high rate of trauma—a true trauma based treatment approach ought also be incorporated. The combination of these types of groups, engagement strategies and structured time will provide the added value of diminishing the level of social isolation to which many of these individuals are prone, and which has been shown to be a risk factor for both violence and recidivism.
*LSCMI • Level of Service/Case Management Inventory*HCR-20 • Historical Clinical Risk ManagementFor more in this series of articles, check….
-
Violence Risk Assessment Seminar & Webinar
Bibliography:
1. Engaging Challenging Patients and Clients: Wood Did It Best: SWEET Institute, 2018
2. Engaging Challenging Patients and Clients: Wood’s Example: SWEET Institute, 2018
3. Engaging Challenging Patients and Clients: When Everything Else Failed: SWEET Institute, 2018
4. De-escalation: 5 Reasons Why Patients Are Likely To Escalate








