Steps to Integrate Substance Use Treatment and Mental Health Services
LEARN MORE, PRACTICE DIFFERENTLY, AND FEEL CONFIDENT WORKING WITH CLIENTS BY JOINING US FOR A SEMINAR ON, “NEW STRATEGIES FOR SUBSTANCE USE ASSESSMENT,” ON FEBRUARY 20, 2019, 9:30AM – 4:30PM
“Raj tells me one thing and his team tells me something else. He and I agreed that we would do one thing, and then his substance use treatment team opposes it and asks him to do something totally different. I don’t know what to do anymore.” Maryann, one of the clinicians on the HOPE ACT team working with Raj, articulated these words to Rodis, the consultant, who looked at her, paused, and said, “Working with different teams can be challenging and frustrating, and it is getting clearer and clearer now that Raj receiving treatment for his substance use elsewhere has not been effective. Let us discuss some steps on how to smooth things out a bit.”
Split treatment remains a challenge and has been shown to be detrimental to our patients and clients. This becomes more significant when it involves a patient population with several comorbidities. Patients with both mental health and substance use treatment needs are particularly vulnerable to split treatment, and integrating substance use treatment and mental health services is not only advised but also essential if we are to make meaningful changes.
In a previous article on integrated care (see Basic Integrated Care Skills for Non-Medical Staff: 5 Reasons Why), I 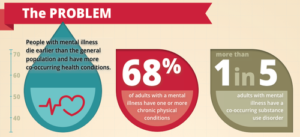 outlined reasons why physical care and mental health care needs must be integrated. These same reasons also apply when considering why it is important to effectively integrate substance use treatment and mental health services. There are, however, specific strategies to use for effective integration of substance use treatment and mental health services, and, as Rodis stated, let us start with some steps that you can use as you work towards integration for the sake of your patients and clients, your career gratification, and your agency. Below are five steps to follow.
outlined reasons why physical care and mental health care needs must be integrated. These same reasons also apply when considering why it is important to effectively integrate substance use treatment and mental health services. There are, however, specific strategies to use for effective integration of substance use treatment and mental health services, and, as Rodis stated, let us start with some steps that you can use as you work towards integration for the sake of your patients and clients, your career gratification, and your agency. Below are five steps to follow.
1. Ask
 I often mention that the clinician who does not know what he or she is looking for does not know what he or she encounters, what to ask, when to ask, and how to ask it. Furthermore, he who asks not may not know or learn. This often leads to missed opportunities for our patients and clients, improper diagnosis, limited treatment, lack of comprehensive treatment planning, and lack of clarity for the next steps after first trial failure. All this also applies to working with patients and clients with substance use disorders. Integrating substance use treatment and mental health services entails all members of the team “asking.” Asking, in turn, requires its own set of strategies, so that it does not lead to feelings of judgment, discrimination, or shame. Asking also requires the right timing, the right flow, and the readiness to move to the next step. When done properly, it is a powerful tool and step in the practice of integration.
I often mention that the clinician who does not know what he or she is looking for does not know what he or she encounters, what to ask, when to ask, and how to ask it. Furthermore, he who asks not may not know or learn. This often leads to missed opportunities for our patients and clients, improper diagnosis, limited treatment, lack of comprehensive treatment planning, and lack of clarity for the next steps after first trial failure. All this also applies to working with patients and clients with substance use disorders. Integrating substance use treatment and mental health services entails all members of the team “asking.” Asking, in turn, requires its own set of strategies, so that it does not lead to feelings of judgment, discrimination, or shame. Asking also requires the right timing, the right flow, and the readiness to move to the next step. When done properly, it is a powerful tool and step in the practice of integration.
2. Assess
In a series of articles on New Strategies to Working with Individuals with Substance Use Disorder, I outlined a total of  ten questions to ask, as part serving and making a difference in the lives of individuals with substance use disorder. They are categorized as:
ten questions to ask, as part serving and making a difference in the lives of individuals with substance use disorder. They are categorized as:
(1) Patterns of use; (2) Triggers to use; (3) Management of cravings;
(4) Explanatory model of use; (5) Escalating factors;
(6) Consequences of use; (7) Comorbidities; (8) Sense of self;
(9) Stage of change; and (10) Purpose and meaning.
When practiced well, these questions allow clinicians with a comprehensive assessment, and can become the cornerstone for working with patients and clients with substance use disorder and an essential and key step to integrating substance use treatment and mental health services.
3. Formulate
I frequently talk about problem solving, that, in order to properly and adequately problem-solve, we need to get to the bottom of the issue. Otherwise, we risk coming up with a solution that may end up engendering more problems than at the start.
frequently talk about problem solving, that, in order to properly and adequately problem-solve, we need to get to the bottom of the issue. Otherwise, we risk coming up with a solution that may end up engendering more problems than at the start.
I also like to explain that the first set of steps to problem solving is problem formulation. What exactly is the problem? How do we frame it? What do we think is causing it? What do we call it? The answers to these questions help ensure that whoever is involved in addressing the problem has a common understanding of what the problem really is. This problem solving process, in particular, problem formulation, is by far the most crucial when integrating substance use treatment and mental health services. Nonetheless, just like the first step of asking, formulating also entails its own set of strategies, and the most comprehensive approach concerning this is the bio-psycho-social and cultural one.
4. Implement 
You have properly asked, adequately assessed, and appropriately formulated, and now it is time to move to the next step—implementing. Similar to the other steps, implementing also has an art and science, but there are steps you can take right now. Paying attention to where the patient and client is at, paying attention to the possible roadblocks, and making sure that the treatment or plan is collaborative, tailored, and stage based, as opposed to front loaded based, are all essential components of implementing.
5. Track
 As you ask, assess, formulate, and implement, you also need to track. After all, this, too, is an essential step in problem solving. What has the process been like? What did we do well? What could we have done and can now be done , differently? What is the next step? These are all part of this tracking. This step also entails paying attention to the progress of our patients and clients, their triggers and stressors. Further, focusing on harm reduction as opposed to total abstinence, allowing you and your patient and client to celebrate the small successes, and helping with positive reinforcement, is an added component of tracking. Lastly, tracking also involves using assertive outreach and the tools of engagement as well as cultural sensitivity, all mentioned in previous articles.
As you ask, assess, formulate, and implement, you also need to track. After all, this, too, is an essential step in problem solving. What has the process been like? What did we do well? What could we have done and can now be done , differently? What is the next step? These are all part of this tracking. This step also entails paying attention to the progress of our patients and clients, their triggers and stressors. Further, focusing on harm reduction as opposed to total abstinence, allowing you and your patient and client to celebrate the small successes, and helping with positive reinforcement, is an added component of tracking. Lastly, tracking also involves using assertive outreach and the tools of engagement as well as cultural sensitivity, all mentioned in previous articles.
And so it went. Five steps:
LEARN MORE, PRACTICE DIFFERENTLY, AND FEEL CONFIDENT WORKING WITH CLIENTS BY JOINING US FOR A SEMINAR ON, “NEW STRATEGIES FOR SUBSTANCE USE ASSESSMENT,” ON FEBRUARY 20, 2019, 9:30AM – 4:30PM
References:
-
WHO Capacity Building for Tobacco Control Training Package 4: Strengthening health systems for treating tobacco dependence in primary care. Geneva, World Health Organization, 2013.
-
Institute of Medicine (IOM) Improving the Quality of Health Care for Mental and Substance-use Conditions. Washington, DC: National Academies Press; 2006.
-
Parthasarathy S, Weisner C, Hu TW, Moore C. Association of outpatient alcohol and drug treatment with health care utilization and cost: Revisiting the offset hypothesis. Journal of Studies on Alcohol. 2001;62 (1):89–97.
-
Weisner C, Mertens J, Parthasarathy S, Moore C, Lu Y. Integrating primary medical care with addiction treatment: A randomized control trial. Journal of the American Medical Association. 2001;286 (14):1715–23.
-
Bachman, K.M.; Moggi, F.; Hirsbrunner, H.-R; Donati, R.; and Brodbeck, J. An integrated treatment program for dually diagnosed patients. Psychiatric Services, 48:314-316, 1997.