Maslow’s Legacy: Elevating Mental Health and Transforming Mental Healthcare

Maslow’s Legacy: Elevating Mental Health and Transforming Mental Healthcare
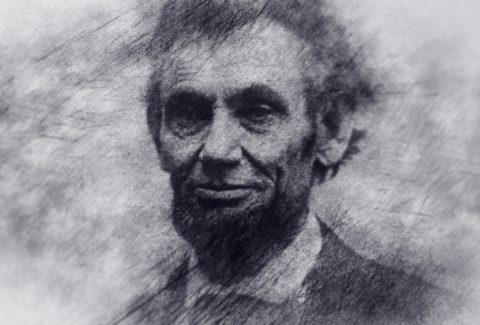
Abraham Maslow[1], a renowned psychologist, left an indelible mark on the understanding of human motivation[2] and well-being through his hierarchy of needs. His insights, though rooted in psychology, extend far beyond academic realms, offering profound implications for mental health and the evolution of mental healthcare.
Maslow’s hierarchy posits that human needs are arranged in a pyramid, starting with basic physiological requirements and ascending to higher-level needs such as self-actualization and transcendence. This framework provides a holistic lens through which we can explore the intricacies of mental health and its intersection with mental healthcare.
Foundations of Well-being:
At the base of Maslow’s pyramid lie fundamental physiological needs[3]—air, water, food, shelter, and sleep. Acknowledging and addressing these basic requirements is foundational to mental health. Access to these essentials forms the cornerstone of a healthy and resilient mind.
Safety and Security:
Maslow’s second tier emphasizes safety and security needs. In the context of mental health, creating environments that foster emotional safety, stability, and a sense of security becomes imperative. Mental healthcare settings must prioritize these factors to provide effective support.[4]
Social Connection:
The third level highlights the importance of social needs. Meaningful connections[5], relationships, and a sense of belonging significantly impact mental well-being. Mental healthcare interventions that incorporate social support systems align with Maslow’s vision for holistic health.
Esteem and Self-Actualization:
The higher tiers of Maslow’s pyramid focus on esteem needs and self-actualization[6]—realizing one’s potential and achieving personal growth. Mental health care should go beyond symptom management to support individuals in their journey toward self-fulfillment and realizing their capabilities.
Maslow’s insights challenge us to move beyond a narrow view of mental health as the absence of illness. Instead, it encourages a comprehensive approach that considers the fulfillment of higher-level needs, promoting a sense of purpose and fulfillment.
In mental healthcare, embracing Maslow’s principles entails tailoring interventions to individual needs, addressing social determinants of mental health, and fostering environments that nurture personal growth. It underscores the importance of a patient-centered approach, recognizing the uniqueness of each individual’s journey to well-being.[7]
In conclusion, the timeless wisdom of Abraham Maslow provides a roadmap for enhancing mental health and transforming mental healthcare. By incorporating his hierarchy of needs into our approach, we can cultivate environments that support holistic well-being, moving towards a more compassionate and effective paradigm in mental health care.
[1] Maslow, Abraham. “Abraham Maslow.” New York (2008).
[2] Navy, Shannon L. “Theory of human motivation—Abraham Maslow.” Science education in theory and practice: An introductory guide to learning theory (2020): 17-28.
[3] Maslow, Abraham. “A THEORY OF HUMAN MOTIVATION The basic needs.” Marketing: Critical Perspectives on Business and Management 2 (2001): 321.
[4] Hayre-Kwan, Surani, et al. “Nursing and Maslow’s hierarchy: A health care pyramid approach to safety and security during a global pandemic.” Nurse leader 19.6 (2021): 590-595.
[5] Rakić, Tomislav, and Snežana Živković. “Hierarchy of needs and correlation connections as an important element of successful employees’ motivation.” Ekonomika 63.4 (2017): 61-73.
[6] Maslow, Abraham. “Self-actualization and beyond.” (1965).
[7] Henwood, Benjamin F., et al. “Maslow and mental health recovery: A comparative study of homeless programs for adults with serious mental illness.” Administration and Policy in Mental Health and Mental Health Services Research 42 (2015): 220-228.