Metabolic syndrome and our patients in the Public Mental Health System

Metabolic syndrome and our patients in the Public Mental Health System
“It’s hard enough to find these people. How can we be expected to screen them for metabolic syndrome, too?”
Maya, the new nurse at the HOPE ACT team, articulated these words to Rodis, the consultant, who then looked at her, paused and responded, “Quite a dilemma.
This is, indeed, one of the most challenging patient populations to work with. The rates of homelessness are high, health literacy rates are low, and the rates of follow-up and commitment to treatment are dismal.
Before making any decision or attempting to problem solve, let us conduct an abbreviated form of a risk-benefit analysis. Let us look at the why.”
It is common knowledge that our patients and clients, particularly those with Schizophrenia, served in the public 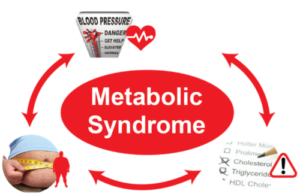 mental health system, have a life expectancy 20 to 30 years lower when compared to the general public. Their level of education is lower, which decreases the likelihood of health literacy. They have financial limitations, which minimizes their choices when it comes to deciding between a healthy meal and bus fare. And, they have substandard living arrangements, which make it harder for them to adequately prepare meals or even store healthy foods. In addition to all this, “It’s hard enough to find them,” as Maya stated, referring to the number of failed attempts by clinicians on the HOPE ACT team and other ACT teams, to meet with the patients. As Rodis said, it is quite a dilemma and a challenge, but one worth exploring, and it starts with taking one step back to look at the why.
mental health system, have a life expectancy 20 to 30 years lower when compared to the general public. Their level of education is lower, which decreases the likelihood of health literacy. They have financial limitations, which minimizes their choices when it comes to deciding between a healthy meal and bus fare. And, they have substandard living arrangements, which make it harder for them to adequately prepare meals or even store healthy foods. In addition to all this, “It’s hard enough to find them,” as Maya stated, referring to the number of failed attempts by clinicians on the HOPE ACT team and other ACT teams, to meet with the patients. As Rodis said, it is quite a dilemma and a challenge, but one worth exploring, and it starts with taking one step back to look at the why.
Below are the reasons why we need to discuss metabolic syndrome in our patients and clients in the public health system. We will start with two reasons, both from the perspective of the patient.
1. Health
As stated above, our patients’ life expectancy is lower when compared to the general population. This is related to their overall health, influenced by a combination of biological and psychosocial factors. They take medications that increase their risk for metabolic syndrome; they have strong genetic predispositions, and they are exposed to stressors in their neighborhoods and their living arrangements, which are associated with and further increase their risk for metabolic syndrome.
There are several additional risk factors. They are much less likely to have a primary care physician, and, if they do have a primary care physician, they are less likely to seek. As a result, they tend to have poorly treated general medical comorbidities and tend to not take their physical health medications. Lastly, they are more likely to have a substance use disorder, which makes follow ups, planning, and adherence more unpredictable.
Social learning and subculture are added factors. For example, our patient population in the public sector tend to be more crisis driven; they are more likely to have executive function difficulties, particularly around planning, and, like all of us, their lifestyle is deeply rooted in strong habits. Their comorbidities do not make it any easier. For example, they are more likely to have a history of trauma, which in turn affects their sense of self, drive, and motivation. The major mental illnesses, like Schizophrenia, Schizoaffective Disorder and Bipolar Disorder, have also been associated with an increased predisposition for metabolic syndrome.
2. Not having a voice
First, do no harm. This principle has been guiding physicians in our work with our patients and their families; it guides  us in our prescribing practices, in minimizing iatrogeny, and in adopting a holistic approach when working with our patients.
us in our prescribing practices, in minimizing iatrogeny, and in adopting a holistic approach when working with our patients.
This principle is also related to our humanistic approach, to always remember that our patients are people, first, and that our mandate is to help them live to their highest possible level of functioning with the least level of risk. During supervision, I tend to ask clinicians to take one step back and ask themselves, “What if this were a friend, a family member, their spouse, child, or their parent; would I do or not do the same for him or her.” I just invite them to do their best to act accordingly. In a world where fairness is elusive, where patients affected with mental illness are stigmatized and discriminated against, it is our responsibility and our duty to be at the table and be that voice for the voiceless. And it starts with our daily practice.
“It’s hard enough to find these people. How can we be expected to screen them for metabolic syndrome, too?”
Maya, the new nurse at the HOPE ACT team, articulated these words to Rodis, the consultant, who then looked at her, paused and responded, “Quite a dilemma. This is, indeed, one of the most challenging patient populations to work with…Let us look at the why.”
 Two reasons why have been discussed, both from the perspective of our patients and clients. The first one relates to our overall patient health, and the second relates to the fact that our patients tend to not have a voice. As we have been called to serve, we ought to continue to strive for comprehensive approach to healthcare for our patients and clients, and also continue to voice for them, while helping them find and use their own voice. This, as already stated, starts with the way we work with them. It is one of the reasons why it is crucial for us to pay attention to metabolic syndrome in our patients in the public mental health system.
Two reasons why have been discussed, both from the perspective of our patients and clients. The first one relates to our overall patient health, and the second relates to the fact that our patients tend to not have a voice. As we have been called to serve, we ought to continue to strive for comprehensive approach to healthcare for our patients and clients, and also continue to voice for them, while helping them find and use their own voice. This, as already stated, starts with the way we work with them. It is one of the reasons why it is crucial for us to pay attention to metabolic syndrome in our patients in the public mental health system.
Thank you for reading this article. What other patient related reasons and/or experiences would you like to share with us? Please contact us. Until soon.
Your friend and colleague,
Mardoche
References:
-
Pollex RL, Hegele RA (September 2006). “Genetic determinants of the metabolic syndrome”. Nature Clinical Practice. Cardiovascular Medicine. 3 (9): 482–9.
-
Poulsen P, Vaag A, Kyvik K, Beck-Nielsen H (May 2001). “Genetic versus environmental aetiology of the metabolic syndrome among male and female twins”. Diabetologia. 44 (5): 537–43.
-
Bouchard C (May 1995). “Genetics and the metabolic syndrome”. International Journal of Obesity and Related Metabolic Disorders. 19 Suppl 1: S52–9.
-
Katzmarzyk PT, Leon AS, Wilmore JH, Skinner JS, Rao DC, Rankinen T, Bouchard C (October 2003). “Targeting the metabolic syndrome with exercise: evidence from the HERITAGE Family Study”. Medicine and Science in Sports and Exercise. 35 (10): 1703–9.
-
He D, Xi B, Xue J, Huai P, Zhang M, Li J (June 2014). “Association between leisure time physical activity and metabolic syndrome: A meta-analysis of prospective cohort studies”. Endocrine. 46 (2): 231–40.
-
Xi B, He D, Zhang M, Xue J, Zhou D (August 2014). “Short sleep duration predicts risk of metabolic syndrome: A systematic review and meta-analysis”. Sleep Medicine Reviews. 18 (4): 293–7.
-
Vancampfort D, Correll CU, Wampers M, Sienaert P, Mitchell AJ, De Herdt A, Probst M, Scheewe TW, De Hert M (July 2014). “Metabolic syndrome and metabolic abnormalities in patients with major depressive disorder: A meta-analysis of prevalences and moderating variables”. Psychological Medicine. 44 (10): 2017–28.